
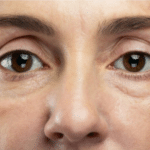
At first, it looks like a bug bite or an ingrown hair. But soon, your child has a red rash that they can’t stop scratching, and it appears to be oozing or crusty and spreading.
The Staphylococcus genus of bacteria includes at least 30 species. Most are harmless and reside on the skin and our mucous membranes. However, several species can cause a wide variety of infections. Staphylococcal toxins are a common cause of food poisoning. Staphylococci can also cause bacterial conjunctivitis.
In the 37 years that I worked as a primary care physician, I saw many forms of severe skin infections. But it wasn’t until around 1990 that a new type of staph suddenly became the most common cause of severe infections.
Methicillin-resistant Staph Aureus (MRSA) is a dangerous invasive gram-positive bacteria. In the 1990s, MRSA became the most common hospital-acquired infection, the most common school-related skin infection, and the most common infection seen in IV drug users. It is resistant to multiple antibiotics and grows rapidly (doubling its numbers every 20 minutes), developing a hard, thickened covering that protects the germ from standard cleaning. The most common phrase I heard when examining a possible early MRSA infection was, “I have a spider bite.” The patient presents with a skin lesion that is hard and red, with a quarter-sized abscess with a central red mark that looks like a bite.
MRSA is easy to bring home and difficult to remove. The germ can live for several days on surfaces. Usually, it is picked up through skin-to-skin contact, but it has been detected on everything from money to exercise equipment. Once picked up, it can become a skin infection, which may be mild or severe. It’s essential to identify it quickly before it can cause severe disease.
A MRSA infection is usually a painful, rapidly expanding abscess (boil) or a red swollen skin wound that looks much worse than a bug bite or rash. The treatment for abscesses or infected wounds is incision and drainage done by a medical provider. Trying to “pop” an abscess may cause the pus to be pushed deeper into the body and cause necrotizing fasciitis, compartment syndrome, or sepsis. Antibiotics help prevent the spread, but the medicines necessary to treat MRSA are frequently harsh. Urgent treatment is needed if there is a fever, a swollen hot joint, an inability to bend a joint, swelling around an eye, or multiple abscesses occurring almost immediately. The infection can be severe in someone who just had surgery, so nearly all pre-op checks include a nasal swab for MRSA.
MRSA infections can cause severe scarring and become more serious when they go deeper into the body, entering the bloodstream, joints, lungs, or heart. Getting treatment quickly is important.
If one family member gets MRSA, assume everyone has some form of it. Hand washing, surface cleansing, and using certain antibacterial body washes plus a week of prescription nasal ointment should prevent further infections and spread. It is also essential to notify outside contacts and schools.
Clean any surfaces the patient has contacted with diluted bleach. Do not share clothing, hats, towels, washcloths, or combs. Stop nose-picking. Avoid allowing scabs to form on wounds as they enable and hide infections.
The best treatment is simple prevention. Teach your family how to wash hands with plenty of soap properly. Instruct them to sing Happy Birthday all the way through while washing.
Disclaimer: The views and opinions expressed on Annapolis Moms Media and its affiliates are those of the authors and/or experts and do not necessarily reflect the official policy or position of Annapolis Moms Media. Any content provided by our bloggers or authors is of their opinion and is not intended to malign any religion, ethnic group, club, organization, company, individual, or anyone or anything.
The published article is available for informational purposes only and is not considered licensed professional advice on any subject matter. By viewing articles/blog posts, the reader understands there is no client relationship between the reader, the publisher, and its authors. The article/blog should not be used as a substitute for professional advice from a licensed professional, and readers are urged to consult their own counsel on any specific questions concerning a specific situation.



 Anne Arundel County Fair
Anne Arundel County Fair 